There are many reasons you might need or choose to express your milk. In this article, we’ll explore different ways to express, how to make it as easy and effective as possible, and how to store and handle your milk safely.
Reasons for expressing
Your approach to expressing will depend on your reasons for doing it. Here are some of the most common situations.
When a baby can’t breastfeed
Babies and mothers have many instincts for breastfeeding, but it is still a learned skill that can take time and practice. When babies won’t breastfeed, it is usually because they can’t. This could be for many reasons, for example:
• they were born early, or very small,
• they had a difficult birth,
• they are sleepy as a result of birth medications,
- they are unwell,
- they have a tongue tie, or it’s taking time to learn how to breastfeed.
Expressing milk when your baby cannot nurse (or nurse effectively) protects your milk supply and provides milk to feed them. Human milk is especially important for babies who are unwell or premature as it helps protect against illness and infections, and is ideal for a baby’s sensitive and immature digestive system. (1)
Expressing milk is often a short-term solution. However, some mothers may find themselves expressing their milk longer-term for a baby who is unable to breastfeed. This is known as ‘exclusive pumping’ (or ‘EP’).
If you’re expressing all of most of your milk, you’ll need an efficient plan for doing it – and as much help as possible. LLL Leaders are on hand with information and encouragement. It’s a huge labour of love.
Making more milk
From a few days after birth, milk production works on a supply and demand basis: the more milk you remove, the more milk you will make. The first two to four weeks are the ideal time to boost your milk supply. If not enough milk is removed during this early period, it can limit how much you’re able to make later. (2)
A small number of women have underlying breast or health conditions that may reduce milk production. (3) But most mothers who are making milk are able to make more, especially if they remove milk early and often after birth. This may mean expressing as well as – or instead of – breastfeeding.
Return to work or study
There are many ways to combine working and breastfeeding. It is not always necessary to express milk when returning to work. It depends on:
- the age of your baby,
- the length of time you are apart,
- how much time and energy you have for expressing milk,
- how easy you find it to express milk (read on for ways to make expressing more efficient!), and
- your baby’s willingness to take your milk when you aren’t there.
At first, you might find that you need to express regularly to keep your breasts comfortable. Many mothers find that their breasts quickly adjust to their new breastfeeding pattern, until they no longer need – or want – to express as often, or even at all. The older your baby, the more flexibility you’re likely to have.
Separation
You and your baby may need to be apart for other reasons, such as exercise, illness, an appointment or event, or a night away. Your baby has an intense need for your presence as well as your milk, and separation can be hard for both of you. Young babies are very portable and often enjoy being out and about. It’s often possible (and easier!) to take your baby with you, perhaps with a carer looking after them nearby.
When you and your baby can’t be together, you can express your milk to keep your breasts comfortable and your milk supply strong. With a little advance planning, you can provide your baby with their usual milk while you’re apart.
Donating milk
Donated human milk helps to save the lives of premature and sick babies. If you have plenty of milk for your own baby you could express extra, donating your surplus milk. You can find out about donating through a milk bank here.
Expressing by choice
Some mothers choose to express milk some or all of the time, rather than breastfeeding. You might want – or feel pressured – to let a partner or other family member feed your baby. If you’re thinking of expressing to make life easier, or to get more sleep, it might be worth exploring other options first. Some choose to exclusively pump because they don’t enjoy breastfeeding, but want their baby to have the benefits of their milk.
There are many ways partners and family can bond and be involved with a baby, and expressing milk takes time and energy. Drinking milk from a cup or bottle isn’t quite the same as feeding at the breast, (4) but any amount of your milk, at the breast or expressed, is valuable for your baby!
How do I express?
Hand expressing
You can express milk without any equipment. Hand expressing is a useful skill to learn for all stages of breastfeeding. It takes a little practice, but can quickly become second nature.
- It is free and can be done any time, anywhere!
- It’s the perfect choice for the early days after birth when you are producing small amounts of colostrum (first milk).
- You might like to hand express some colostrum during the last few weeks of pregnancy. It’s good practice, and helps you become familiar with your breasts. Colostrum collected during pregnancy can be fed to your baby after birth, especially if you are separated, or if they need extra milk.
- Using your hands during a pumping session can help you get more milk. See ‘Expressing Tips’ below.
- Hand expressing is a reliable backup for emergencies like a pump failure, power cut, or unexpected separation from your baby.
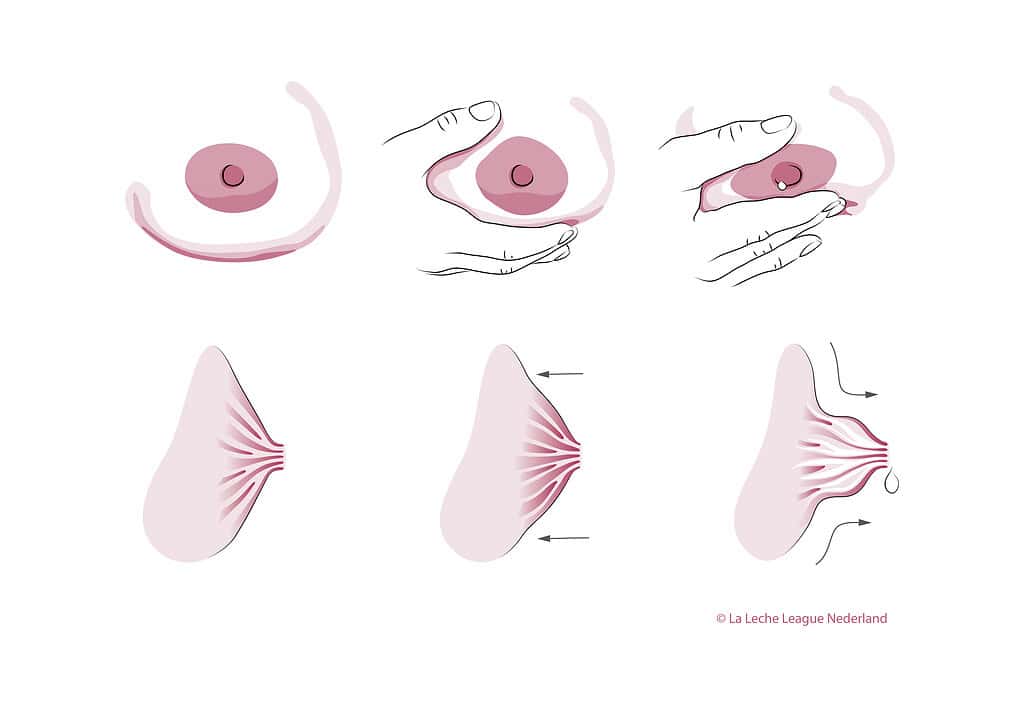
Thumb and fingers in one movement towards the chest, towards each other, and towards the nipple.
You can find hand expressing videos in Further Reading and Resources, below.
If you need to express frequently, for example to increase your milk production, or to provide all or most of your baby’s milk, then you’ll probably want to use a breast pump.
Pumping milk

A. Manual breast pump
B. Single electric pump
C. Double electric pump
What kind of pump do I need?
Many different kinds of pumps are available to hire or to buy. The best pump for you depends on your reason for expressing and your personal preference.
- Single manual or electric pumps are best suited to occasional expressing, for example, short-term separation or returning to work when your baby is older. They can also be useful for expressing ‘to comfort’ whenever your breast feels very full and your baby doesn’t want to nurse.
- Double electric pumps express milk from both breasts at once, which saves time. This may be especially useful if you need to express often. Double pumping may also increase milk production more effectively than single pumping. Double pumps come in various sizes.
- Hospital grade pumps are larger, more powerful double pumps, intended to be used multiple times a day, and by more than one person. They are usually hired. This may be the best kind of pump for you if you’re exclusively expressing, or expressing intensively to increase milk production. Once your supply has settled at a stable level, you might find you can switch to a smaller pump.
- Hands-free (wearable) pumps can be handy if you want to pump on the go, or pump and multitask. If you need to express a lot of milk you might find that this kind of pump isn’t enough by itself, but it can be a useful extra. Wearable pumps can be held in place by a standard bra. It’s also possible to make or buy a ‘hands-free’ pumping bra to hold a conventional pump.
- Squeezy silicone ‘milk collectors’ tend to be best suited to occasional expressing. They can be used to collect milk that drips from one breast while you nurse on the other, or gently squeezed to encourage milk to flow. Using them a lot can result in oversupply (producing more milk than you need).
What else do I need to know about pumps?
Pump fit
Pumps are often sold in a standard size, however pump parts come in different sizes. The funnel-shaped piece that touches your breast is called a flange, or breast shield. The tubed-shaped bit that the nipple goes into is called the nipple tunnel.
If pumping is painful or causes swelling and/or rubbing, you may need a bigger or smaller flange. Sometimes different flange sizes are needed for each breast.
Your nipple should be snug, but have enough room to slide in and out a bit during pumping, without rubbing. The areola (darker area around your nipple) may move slightly with it, but it shouldn’t be drawn into the nipple tunnel. After pumping, your nipple will probably be bigger, but shouldn’t seem darker or swollen.
Experiment to see what works best. The best fit for you will be completely comfortable and give you the most milk.
Suction strength and cycle speed
Electric pumps often come with a range of settings, including suction strength and for cycle speed.
A pump is trying to mimic a breastfeeding baby. When a baby nurses, they start with fast, light sucks to trigger a milk release (‘letdown’). Once the milk is flowing they switch to deeper, slower sucks.
- You might begin by using a low suction, high speed setting (sometimes called ‘stimulation mode’).
- Once your milk starts flowing, you can switch to a higher suction, lower speed setting.
Exactly how high or low depends on how it feels and how well milk is being removed. A pump usually provides most milk when it is set at the highest suction level that still feels comfortable. (5)
Painful pumping may reduce milk flow, damage your nipples, and is unlikely to make you feel like doing it!
How often and when should I express?
If your baby can’t breastfeed yet, aim to express 8–10 times in a 24-hour period. (6) These do not need to be at regular time intervals, but avoid gaps longer than 6 or 7 hours. (7) After the first month, once your supply is well established, you may find that you can get enough milk with fewer sessions. (8)
If you are trying to make more milk, express after or between feeds. How often depends on how much more milk your baby needs, and how feeding at the breast is going. Lots of short, frequent expressions (even five or ten minutes here and there) may be more effective for increasing milk production than fewer, longer sessions.
If you are returning to work or study, how often you express will depend on the age of your baby, how long you’ll be away, and how your breasts feel. Aim to keep your breasts comfortable and (if your baby accepts expressed milk) to express as much in total as your baby is likely to drink. Nurse as much as possible when you’re together, to keep your supply strong.
If you are stockpiling milk for short-term separation or in the run up to a return to work, you could express once or twice a day, after or between feeds. If your baby typically feeds from one breast, you could express from the other side while they feed. The amounts may seem small, but they quickly build up!
If you’re expressing milk to donate, it can help to follow a regular pattern, for example, expressing once a day or every couple of days at around the same time. You might want to check how often the milk will be collected (or when you can drop it off) and how long you have to reach the target amount, if there is one.
How long should I express for?
Just like breastfeeding, expressing milk is not a ‘one-size-fits-all’. Observe your milk flow, notice how your breasts feel, and find what works for you.
- If you are using a single pump, a thorough expression usually takes about 20 – 30 minutes for both breasts. You might try switching sides every few minutes, when the milk flow slows.
- Double pumps save time. A double-pumping session that replaces what would have been nursing will probably last no more than 15 minutes. However, it is more important to pay attention to your breasts than the clock.
How much milk will I express?
How much you can express at any one time depends on lots of different things. If you’ve never used a pump before, it might be helpful to think of the first few pumping sessions as practice.
- In the first 24 hours after birth, you’re likely to get small amounts each time (from a couple of drops to a teaspoonful). Expect the amount to increase every day in the next week or so – you’re ‘putting in your order’ for more milk later. (9, 10)
- Expect to express different amounts at different sessions: from 15ml (1/2 oz) to 90ml (3 oz) or more, depending on the time of day, when you last nursed or expressed, and how you’re feeling. Notice the times of day (or night) when you get most milk – it may be easiest to express then.
- Once milk production peaks, a typical feed is about 60 – 120ml (2 – 4oz).
If you are exclusively pumping, it might be helpful to know that full milk production for one baby can be anything from about 440 – 1300ml (25 – 44 oz) in 24 hours. The average is around 750 – 800ml (26 oz). (11)
Being able to express 650ml – 750ml in 24 hours by 2-3 weeks after birth gives you a very good chance of making all the milk your baby will ever need. (6, 12) Milk production reaches its peak by about one month after birth, and stays relatively stable until around six months. (13)
We all respond differently to pumps. How much you can express is not always a reliable or accurate sign of how much milk is there. It’s important to remember that a baby who is nursing effectively will get more milk than a pump.
Expressing tips
Before expressing:
- Wash your hands and get comfortable.
- Put something warm on your breasts, such as a warm flannel.
- Gently massage your breasts.
- Use any objects or techniques that help you to feel calm and relaxed, such as music, deep breathing, or visualisation.
While expressing:
- Try ‘hands-on pumping’ to help increase the amount of milk.
- Use breast compressions to increase milk flow.
- Take a break midway and gently massage your breasts to help increase the amount of milk.
- Try nursing your baby on one side and expressing on the other, or expressing from both sides at the same time, to encourage more milk releases.
After expressing:
- Hand express for a minute or two to see if you can get a bit more milk – this can be especially helpful if you’re trying to boost milk production.
Cleaning pump parts
- There isn’t complete agreement about cleaning pumping equipment. Some public/advisory bodies (including NHS England) recommend sterilising equipment after every feed. (14)
- Others recommend washing pump parts thoroughly after every feed and sterilising once a day. (15)
- Some advisory bodies and breastfeeding organisations state that pump parts do not need to be sterilised, and that washing in hot soapy water (or a dishwasher) is enough if your baby is healthy and full term. (16)
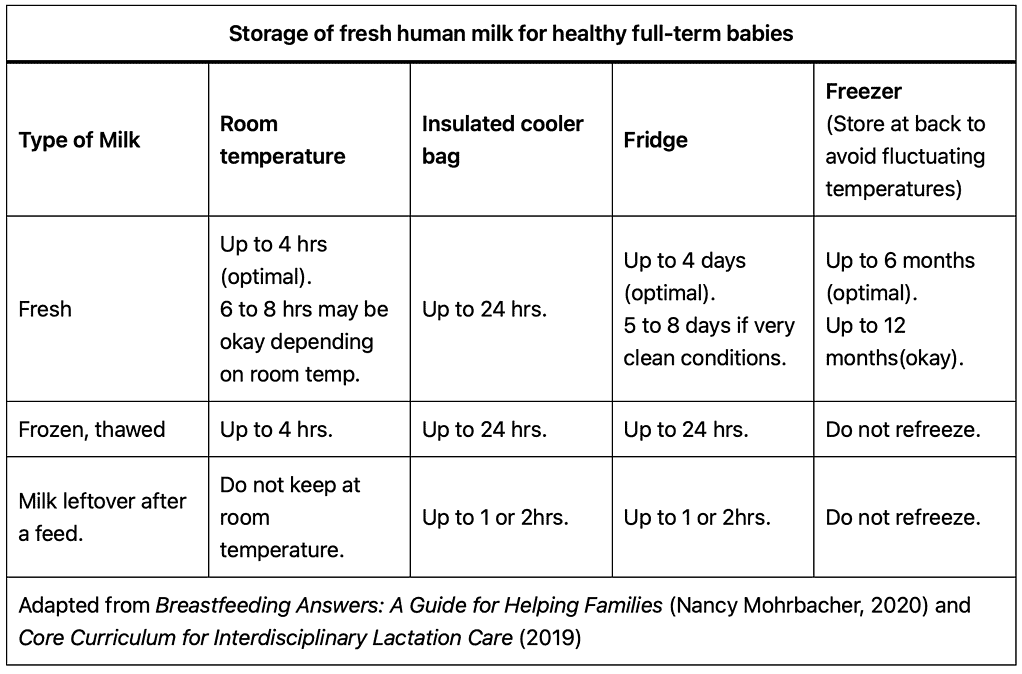
Day-to-day milk handling
- There is very little research on the day-to-day problems of milk handling, so guidelines often err on the side of caution. (17)
- Fresh human milk kills almost all bacteria, viruses, and fungi that it comes in contact with. (18, 19)
- Mothers who are exclusively pumping, or expressing frequently, sometimes put the whole pumping kit (flanges attached) in a clean container in the fridge until the next expressing session and clean everything at the end of the day.
- Human milk can be safely stored at room temperature for 4 hours (see below). Some parents apply the same timeframe to their pump and pump parts, and express multiple times within a 4 hour period before cleaning everything.
- One quick method of sterilising is to use a sterilising fluid that you change every 24 hours. Submerge pump parts in the solution after washing them each time.
Washing and drying
- Ensure hands and pump area are clean.
- You may like to use a separate basin and separate utensils for cleaning pump parts and equipment, rather than the sink.
- Clean with hot soapy water and rinse separately with clean water.
- Some pump equipment is also dishwasher-safe.
- Air dry or dry with paper towels.
- Clean pump dials and switches with a disinfectant spray or wipe.
- Store dry pump equipment in a clean container.
If you are expressing milk for a sick or premature baby, good hygiene is even more important. Your hospital or milk bank may have its own guidelines.
Storing Milk
How long can I store milk for?
- There isn’t complete agreement about milk storage.
- Wherever you are storing milk, the fresher it is, the better.
- Good hygiene is important — clean hands, clean pump parts, clean storage.
Combining expressed milk
When combining milk expressed at different times, mix cold with cold:
- Chill newly expressed milk before adding it to an existing container.
- You can add refrigerated milk to frozen as long as there is less refrigerated milk than frozen.
- Use within the time limit of the oldest expressed milk.
What can I store milk in?
- You can store milk in any clean container, such as a hard (BPA-free) plastic or glass container with a tight-fitting lid, or a milk storage bag (disposable or silicone). (20, 21)
- Milk expands in the freezer, so leave space in the bag or bottle if you plan to freeze it.
- Put the date on the container.
How much milk should I store?
- Store milk in small quantities to avoid waste. Small amounts also defrost more quickly.
- For babies older than one month, a feed is approximately 60 – 120ml.
How do I prepare stored milk?
- You don’t have to warm milk – some babies like it cold!
- If you do warm milk, run the container under a warm tap or place it in a pan of warm water.
- Never use a microwave or heat milk directly.
- Swirl milk to combine rather than shaking it.
- If defrosting milk, thaw it overnight in a fridge or hold it under warm running water.
- Thawed milk should not be kept at room temperature. It should either be fed immediately or put in the fridge.
Smelly milk
Sometimes milk smells or tastes soapy after a short time in the fridge or freezer. This is because of an enzyme (lipase) that breaks down fats in milk. The milk is completely safe and most babies will drink it. However, if they refuse to, heat freshly-expressed milk to scalding (bubbling around the edges, but not boiling) and then quickly cool and freeze it. Scalding reduces some of the immune factors, but may be the only option for some families. (22)
You can also experiment with the length of storage time needed for the milk to acquire the smell. Some babies will accept smelly milk mixed with fresh milk.
Summary
- There are many reasons you might need or want to express your milk.
- How you express, and how often, depends on why you are doing it.
- Hand expressing is a useful skill for anyone who is breastfeeding.
- If you need a lot of milk, you’ll probably want to use a double electric pump.
- There are lots of things you can do to make expressing milk comfortable and efficient.
- It’s important to follow good basic hygiene practices, though guidelines vary.
Written by Charlotte Allam and Jayne Joyce, November 2025.
Review due November 2027.
Further Reading and Resources
From our website
Antenatal expression of colostrum
Breastfeeding your premature baby
Exclusively pumping breastmilk for your baby
How to increase your milk supply
My baby needs more milk (includes a description of breast compressions)
Oversupply (too much milk)
Other resources
- The Art of Breastfeeding, 9th edition (La Leche League International, 2024), chapter 15
- Academy of Breastfeeding Medicine Clinical Protocol #8: Human Milk Storage Information for Home Use for Full-Term Infants, Revised 2017. Available at bfmed.org
- Breastfeeding Answers, by Nancy Mohrbacher (Nancy Mohrbacher Solutions, 2020), chapter 11
- Making More Milk, by Lisa Marasco and Diana West (McGraw Hill, 2019)
- Relactation: A Guide to Rebuilding Your Milk Supply, by Lucy Ruddle (Praeclarus Press, 2020)
Flange fit
Milk donation
Hand expression videos
The first few days: firstdroplets.com
At any stage of breastfeeding: unicef.org.uk/babyfriendly/baby-friendly-resources/breastfeeding-resources/hand-expression-video/
Credit for illustrations: Brigitte Sparnaaji, from Breastfeeding Illustrated, published by La Leche League GB, 2021. Copyright Stichting La Leche League Nederland
References
- Lokossou, Gatien A G et al. “Human Breast Milk: From Food to Active Immune Response With Disease Protection in Infants and Mothers.” Frontiers in immunology vol. 13 849012. 5 Apr. 2022, doi:10.3389/fimmu.2022.849012
Available at https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.849012/full (accessed October 28 2025).
- Kent JC, Gardner H, Geddes DT. Breastmilk production in the first 4 weeks after birth of term infants. Nutrients. 2016;8(12):756. https://doi.org/10.3390/nu8120756
Available at https://www.mdpi.com/2072-6643/8/12/756 (accessed 28 October 2025)
- Geddes DT et al. “Risk Factors for Low Milk Production”. Proceedings. 2023; 93(1):17. Available at https://doi.org/10.3390/proceedings2023093017 (accessed 13 October 2025).
- Cudziło, Dorota et al. “Infant and baby feeding and the development of the maxillofacial complex based on own observations and the literature.” Developmental period medicine vol. 22,3 (2018): 255-259. doi:10.34763/devperiodmed.20182203.255259
Available at https://pmc.ncbi.nlm.nih.gov/articles/PMC8522884 (accessed 28 October 2025).
- Geddes, Donna Tracy et al. “25 Years of Research in Human Lactation: From Discovery to Translation.” Nutrientsvol. 13,9 3071. 31 Aug. 2021, doi:10.3390/nu13093071
Available at https://pmc.ncbi.nlm.nih.gov/articles/PMC8465002/
(accessed 13 October 2025).
- UNICEF UK, FM E. The evidence and rationale for the UNICEF UK Baby Friendly Initiative standards. 2013, p. 104.
Available at https://www.unicef.org.uk/babyfriendly/wp-content/uploads/sites/2/2013/09/baby_friendly_evidence_rationale.pdf (accessed 28 October 2025).
- Lai, Ching Tat et al. “Short-term rate of milk synthesis and expression interval of preterm mothers.” Archives of disease in childhood. Fetal and neonatal edition vol. 105,3 (2020): 266-269. doi:10.1136/archdischild-2018-316551
Available at https://pmc.ncbi.nlm.nih.gov/articles/PMC7363781/?utm_source=chatgpt.com (accessed 28 October 2025).
- Levene, Ilana et al. “The relationship of milk expression pattern and lactation outcomes after very premature birth: A cohort study.” PloS onevol. 19,7 e0307522. 29 Jul. 2024, doi:10.1371/journal.pone.0307522
Available at https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0307522 (accessed 13 October 2025).
- Nyamagoudar, Anita H et al. “Retrospective analysis of volumes of manually expressed colostrum among healthy postnatal mothers at a tertiary care referral unit in South India. Not enough milk or not enough patience?.” BMJ paediatrics open vol. 8,1 e002622. 18 Oct. 2024, doi:10.1136/bmjpo-2024-002622
Available at https://pmc.ncbi.nlm.nih.gov/articles/PMC11492951/pdf/bmjpo-8-1.pdf (accessed 13 October 2025).
- Kato, Ikuko et al. “The Trajectory of Expressed Colostrum Volume in the First 48 Hours Postpartum: An Observational Study.” Breastfeeding medicine : the official journal of the Academy of Breastfeeding Medicine vol. 17,1 (2022): 52-58. doi:10.1089/bfm.2020.0366
Available at https://www.researchgate.net/publication/354647562_The_Trajectory_of_Expressed_Colostrum_Volume_in_the_First_48_Hours_Postpartum_An_Observational_Study (accessed 27 October 2025).
- Kent, J.C. et al. Volume and Frequency of Breastfeedings and Fat Content of Breast Milk Throughout the Day. Pediatrics, 2006; 117 (3): e387-e395.
Available at https://www.researchgate.net/publication/7266502_Volume_and_frequency_of_breastfeeds_and_fat_content_of_breastmilk_throughout_the_day (accessed 13 October 2025).
- Levene, Ilana et al. “The relationship of early expressed milk quantity and later full breastmilk feeding after very preterm birth: A cohort study.” Maternal & child nutrition vol. 21,1 (2025): e13719. doi:10.1111/mcn.13719
Available at https://onlinelibrary.wiley.com/doi/full/10.1111/mcn.13719 (accessed 13 October 2025).
- Rios-Leyvraz, Magali, and Qisi Yao. “The Volume of Breast Milk Intake in Infants and Young Children: A Systematic Review and Meta-Analysis.” Breastfeeding medicine : the official journal of the Academy of Breastfeeding Medicine vol. 18,3 (2023): 188-197. doi:10.1089/bfm.2022.0281
Available at https://www.researchgate.net/publication/368424755_The_Volume_of_Breast_Milk_Intake_in_Infants_and_Young_Children_A_Systematic_Review_and_Meta-analysis (accessed 27 October 2025).
- Scott H, Sweet L, Strauch L, Muller A. Expressed breastmilk handling and storage guidelines available to mothers in the community: a scoping review. Women Birth. 2020;33(5):426–32. https://doi.org/10.1016/j.wombi.2019.09.009
- Salcedo, Jaime et al. “Human milk bactericidal properties: effect of lyophilization and relation to maternal factors and milk components.” Journal of pediatric gastroenterology and nutrition vol. 60,4 (2015): 527-32. doi:10.1097/MPG.0000000000000641
Available at https://repositorioinstitucional.ceu.es/entities/publication/ff0908e2-acd7-4e0c-a4b6-d10cc3998110 (accessed October 28 2025)
- Morniroli, Daniela et al. “The Antiviral Properties of Human Milk: A Multitude of Defence Tools from Mother Nature.” Nutrients vol. 13,2 694. 22 Feb. 2021, doi:10.3390/nu13020694
Available at https://pmc.ncbi.nlm.nih.gov/articles/PMC7926697 (accessed 28 October 2025)
- Trasande, Leonardo et al. “Food Additives and Child Health.” Pediatrics vol. 142,2 (2018): e20181408. doi:10.1542/peds.2018-1408
Available at https://publications.aap.org/pediatrics/article/142/2/e20181408/37584/Food-Additives-and-Child-Health (accessed 29 October 2025)
- Eglash, Anne, and Lori Simon. “ABM Clinical Protocol #8: Human Milk Storage Information for Home Use for Full-Term Infants, Revised 2017.” Breastfeeding Medicine, vol. 12, no. 7, 2017, pp. 390–395. doi:10.1089/bfm.2017.29047.aje.
Available at https://abm.memberclicks.net/assets/DOCUMENTS/PROTOCOLS/8-human-milk-storage-protocol-english.pdf (accessed 29 October 2025)
- Breastfeeding: A Guide for the Medical Profession, by Lawrence, R.A., and Lawrence, R.M. 9th edition, 2022.
