November 2013: My first baby is finally here, and I am over the moon. But I am also leaving the hospital with formula forced upon me and already combination feeding 24 hours after a long, medicated birth. The midwives’ comments about the size of my breasts and the flatness of my nipples floating in my head, I feel my body may well let me down… again.
I had finally been diagnosed with PCOS (polycystic ovary syndrome, a hormonal disorder) just three years earlier, and while I felt relief at finally having a name to put to the symptoms I had been experiencing for over 20 years (weight fluctuations, irregular and painful periods, excess hair), I also knew the diagnosis could well crush my dreams of having children of my own. Getting pregnant was far from straightforward but it did work out in the end. Yet, as soon as our baby girl was here, I started doubting my body’s ability to produce milk. Why was that?
I realise now that from the very first time I spoke to a midwife at my booking appointment, my antenatal appointments focused a lot on the reduced options available to me because of the combination of my age and my size. I had managed to lose nearly four stone in the 18 months following my PCOS diagnosis by taking a combination pill, following a low carb diet and putting myself through a gruelling fitness regime. But that weight started creeping back on as soon as I came off the pill and we started actively trying for a baby, even though my diet was still restricted and I was still exercising regularly.
By the time I had a positive pregnancy test 13 months later, I was in my late thirties and my BMI (body mass index) was nearly back to where it had been in 2010, placing me firmly in the “obese” category again.
So, at that booking appointment, just like any other woman my size and age would be, I was put on the red pathway, which comes with a whole list of warnings of what a BMI of over 30 may mean. There is an increased risk of having a miscarriage, giving birth early, having a big baby or having a stillbirth. The list goes on, with increased risk of thrombosis, gestational diabetes, high blood pressure, pre-eclampsia. Thus the recommendation: a labour-suite delivery instead of access to a midwife-led unit or a home birth because of the increased likelihood of induction of labour, caesarean birth, anaesthetic complications and wound infections. The likelihood of a longer labour and the need for medical intervention were also a factor. Add to that the fact – rather too eagerly shared by one of the midwives “just to warn me” – that 30% of women with PCOS struggle with establishing breastfeeding and you can see why I was already doubting my body on that cold November evening, less than 24 hours after our baby was born.
Fast forward a few days. Despite a little bit of jaundice, the day five weigh-in goes well; my baby has only lost 2% of her birth weight. The midwife beams at me and says, “Whatever you’re doing, it’s working, so just go on doing that.” I smile back at her, glad that my baby is okay, but I don’t tell her the truth: that my nipples are on fire; that I shudder at the thought of bringing the baby to my breast again; that I can’t seem to find a comfortable position. I don’t tell her that I doubt my body, curse the shape of my breasts and my oversensitive nipples, and that I have already started using nipple shields and a pump.
The pain is getting worse at each feed, so I pump more and more. The reason my baby has not lost a lot of weight is due to the fact that I am triple feeding — feeding her at the breast, then using a horrible pump (that doesn’t fit my shape, as I’ll find out later, and makes me even more sore) to top her up with my own milk and, when I don’t have any left, I top her up with an ounce of formula. More often than not she will throw the formula straight back up again, but I am still convinced that my body is failing me and my baby, convinced that she needs the formula to thrive.
Over the next few weeks I continue triple feeding my baby, swapping the thin nipple shields out for the thickest I can find, and investing in an electric pump. I always bottle feed my girl when out and about, with either expressed milk or formula, because I am so body conscious. I simply cannot imagine having to bare my entire breast in front of anyone to fix the nipple shield and then try and latch my baby while sitting in an unfamiliar chair.
I meet my friend Luisa for coffee, and soon I am holding a crying baby while frantically checking a baby bottle in a mug of cold water. It’s a bottle of expressed milk which the cafe staff have overheated. “Will you not just put her on?” she asks gently, as she sits there, effortlessly nursing her older baby. I can’t. I don’t even bring my nipple shields when I go out at this stage. At the end of that meet-up Luisa tells me again about the local LLL group. And when my little girl is about six weeks old, I go to my first LLL meeting.
It was a struggle to get out of the house but, once at the venue, looking around I see a good range of body shapes and sizes, some similar to mine. Everyone is so friendly and so open about their struggles at the same time. I fed my girl in the car, so I’m pretty certain she won’t need a feed during the meeting.
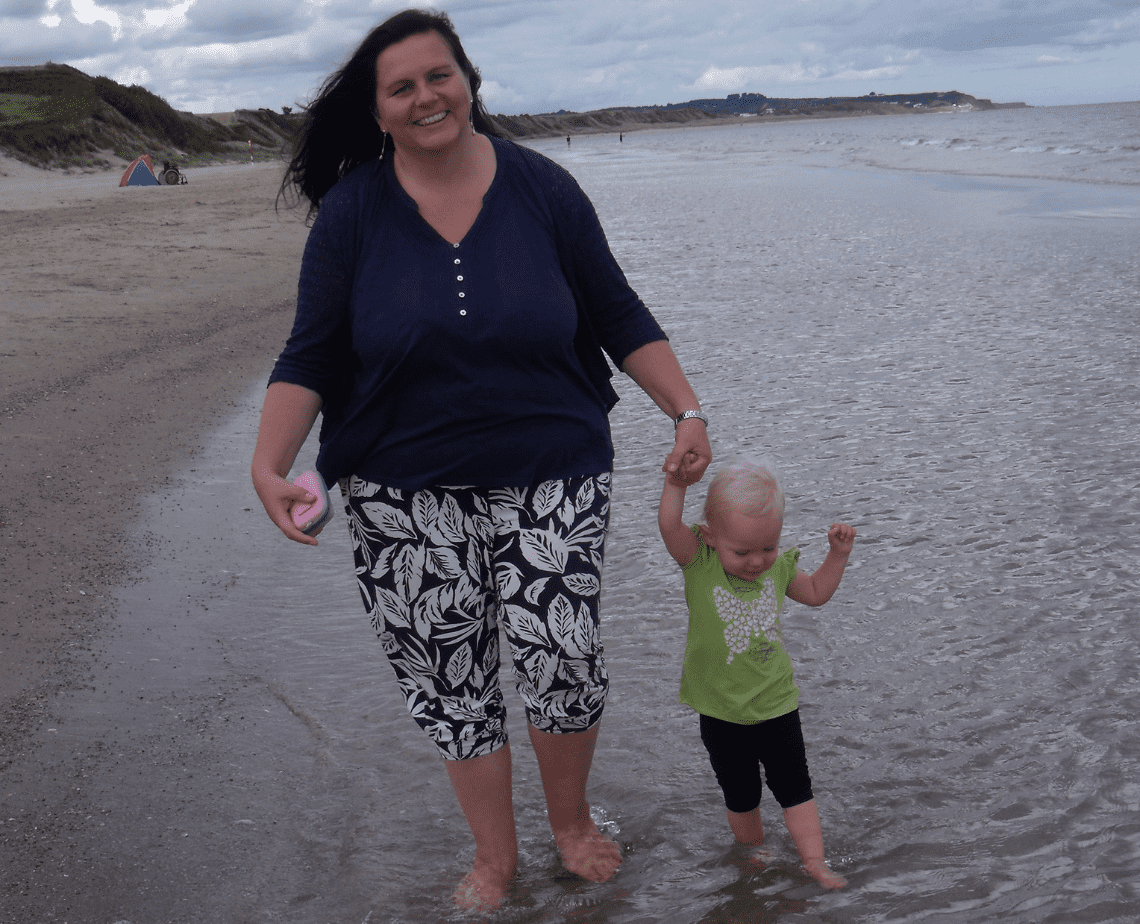
By the end of that meeting, I have decided I am more than a statistic. I’ve just seen three or four bigger women at that meeting feeding their babies without inhibition. One mum, Emma, has just set up her sling library and seeing her carrying her slightly older baby is liberating: this is what carrying a baby in a sling for someone like me may look like. I haven’t yet dared put my little girl into a wrap as I have been so afraid my huge breasts were going to smother her. Another mother tells us about how she relactated after falling seriously ill and, as I walk out of that meeting, I am suddenly determined to do better – to do better for my daughter and for myself.
That first meeting did wonders for my confidence. I asserted myself with my GP, insisting on getting my prolactin levels checked and was subsequently prescribed Domperidone. Within another two weeks I had plenty of milk. We dropped formula completely, and I pumped less and fed more at the breast, still using nipple shields. By the time my little girl was three months old, we had even dropped the shields. We fed for three and a half years and I’m still feeding my second who turned four in August.
Second time round, I did not have a single issue – and donated more than 30 litres of my milk to the Scottish Milk Bank. That first time round, I had lower levels of prolactin due to PCOS, and the prolonged labour, medicated birth and blood loss had a further effect on my milk supply in the early days, and latching issues caused quite severe nipple damage. Second time round, I had a quick labour, a baby with the gentlest latch and, perhaps most importantly, the knowledge that my body had nourished a baby before.
Obesity is, without a doubt, a complex issue, and I do not want to dismiss the consequences an elevated BMI can have on our health. Statistically speaking, pregnant high-BMI women are exposed to the long list of risks mentioned earlier. Statistically speaking, PCOS may have an impact on lactation. But I am not a statistic. None of us are. We all deserve to have health professionals and peer supporters meet us “where we’re at right now”, to work with us, the reality of our lives, the reality of our bodies – and to simply hear us in order to offer support that is tailored to each one of us. In my current role as an LLL Leader, I hope that I do just that for everyone in our antenatal classes and local meetings.
By Marion Dalvai, LLL Fife and Tayside